Professore Associato
Sapienza

In collaboration with: Luca Renzi, Rosaria Laporta, Michail Sorotos
Introduction
The goal of breast reconstruction is to restore the breast's volume and shape (www.ricostruzionemammaria.it). Scientific studies have demonstrated that this operation has no negative influence on cancer evolution. Moreover, it can be said, that if it is not performed correctly, breast reconstruction can have a negative effect, while on the other hand if it is done properly, it can have a positive influence on the psychological balance, the immunologic defenses, and therefore on the life expectancy and the quality of life of the patient. Women whose breast have undergone a surgical amputation (mastectomy) or are congenitally absent due to a developmental anomaly (amastia), are candidates for this operation. There are various techniques available, but the ideal one for each patient is the one discussed and agreed on during the patient's first visit. There are various methods of "breast reconstruction", each one of which has diverse indications depending on various factors that are:
Patient condition:
-
ASA index
-
Type of defect:
-
monolateral
-
bilateral
-
glandular-cutaneous
-
glandular
-
Controlateral breast:
-
small
-
medium
-
large
-
Radiation therapy
-
Autologous tissues available
-
Patient preferences:
-
fear of breast implants
-
reluctant to have accessory scars
-
simplicity of operation
-
symmetrization of the controlateral breast
History
The modern age of breast reconstruction begins during the sixties, with the introduction by Cronin and Gerov of the silicone gel filled implants.
Between the end of the seventies and the beginning of the eighties the development of the tissue expansion technique by Radovan has helped refine more the possibility of breast reconstruction by means of the expanders, which take advantage of the elastic properties of the tissues when they undergo various grades of tension.
During the eighties Becker introduced the permanent expanders avoiding thus the necessity to substitute the temporary expander with a breast implant.
During the nineties, the history of breast implants was strongly influenced by the famous controversy that started in the USA, where it reached its peak in 1992, due to the decision by the FDA (Food and Drug Administration) commissioner David Kessler to forbid the use of silicone gel-filled breast implants, unless in a controlled and restricted mode during clinical trials. Kessler's decision has been published in famous editorial, in which the author explained that his decision was based on the lack, after 30 years of uncontrolled use, of clinical studies that could prove the efficacy and tolerance of the silicone gel-filled breast implants.
The moratorium on the silicone gel-filled implant use has stimulated the development of alternative filling materials and also the studying of the short- and long-term effects of the silicone gel. Both the FDA and the IOM (institute of medicine) in 1999 published a report where it was demonstrated that there was no link between breast implants and the development of cancer, autoimmune diseases, neurological problems or any other systemic disease.
In Europe, the controversy contributed to the publication of the 93/42 EEC act, which came into force on the 15th of June 1998, after a three-year transition period (95-98). According to this act, the implants were moved to the second group of medical and surgical material. In 04/02/03, the European commission has adopted the act 2003/12, putting breast implants in the 3rd Class, thus demanding a more complex process in order to obtain the certificate of conformity.
Iginio Tansini, in 1897, was the first to use the technique of the tranfer of the Latissimus Dorsi muscle from the back along its rotation axis anteriorly, for the repair of the tissue defects of the anterior thoracic wall created after the amputation of the breast. During the twentieth century this technique was widely applied for the prevention of lymphedema following an extended radical mastectomy and for the correction defects of the anterior thoracic wall due to removal of chondrosarcomas.
At the end of the seventies, with the evolution of the knowledge concerning the cutaneous vascularization, Mc Craw proposed the use of a myocutaneous flap. In 1977, Bostwick described extendedly the technique and its indications, reporting his experience with 52 patients during a 2-year period, using the muscle or myo-cutaneous flap togehter with breast implants. His technique, although deviating little from the ones described previously, permits the achievement of a satisfying symmetry with the controlateral breast, by the recreation of the breast's profile. The popularity of this flap was partially obscured by the introduction of the myo-cutaneous Rectus Abdominis muscle flap, but in any case it still remains a valid option in selected patients. The further development of the technique recently, permits in some cases the use of the myo-cutaneous Latissimus Dorsi flap prepared with an "extended" technique and without the use of breast implants.
Among the many authors that have investigated the possibility of breast reconstruction with autologous tissues, Holmström was the first that clinically demonstrated the possibility of using the abdominal skin, by transferring in two patients an extended flap of abdominal skin from the inferior quadrants, using the Deep and Superficial Epigastric vessels.
Later on Hartrampf studied the use of the same flap, but pedicled on the Superior Epigastric Arteries, taking advantage of the intramuscular anastomosis between the systems of the Superior and Inferior Epigastric vessels. Starting in 1979, after the accurate studies of Boyd on the relationship of the vascular systems of the abdominal wall (epigastric vessels, superficial, deep, superior, inferior, circumflex iliacs), the "TRAM" flap, both pedicled and free, became a fundamental tool of the breast reconstruction with autologous tissue.
In 1989 Koshima demonstrated clinically the possibility to overcome the disadvantages of this flap by raising an extended flap of abdominal skin without the Rectus Abdominis muscle but pedicled only on one perforator artery, the "DIEP" flap. Allen was the first that in 1994 used the DIEP flap for breast reconstruction confirming the advantages previously described by Koshima.
During the last ten years various authors have described their experience in the use of the DIEP flap for the reconstruction of the breast. The refining of its surgical technique, the exact definition of its indications and the relationship between cost and benefits has replaced the TRAM flap in cases where the use of muscle tissue is not needed.
topEpidemiology
Currently breast cancer is considered the most frequent cancer in women, with a prevalence of 1.117 of 100.000 people. When it is necessary to perform a mastectomy, the reconstruction is now considered an integral part of the oncologic treatment; numerous evidences demonstrate in fact that such method does not interfere neither with the course of the underlying disease nor with the eventual adjuvant therapies (chemotherapy, radiotherapy); they are moreover noted the positive psychological effects and the oncologic safety of this treatment.
topClinical features
Basically, there are three methods of breast reconstruction, those that reconstruct the breast volume with autologous tissue, the ones that use implants and finally those that use both.
Autologous tissues
The method that includes the use of autologous tissues have the advantage that they offer the reconstruction of a very natural neo-breast since it is made of adipose tissue and therefore with physical characteristics very similar to the controlateral one. Moreover, they offer the creation of an adequate inframammary fold and of a breast volume often completely similar to the controlateral one, eliminating the need of symmetrization with the other breast. Another advantage is that by non-making use of any implants, it permits the treatment by radiotherapy post-operatively, although it must be taken into consideration that this can lead to a loss of the symmetry. Finally, even though these operations have long operating times and longer hospital stays, they offer a reduction of the health costs, since they reduce the number of the eventual surgeries, it is avoided the cost of the breast expander and of the implant and there are avoided the added costs due to the any eventual complications of radiotherapy. The flaps raised from the abdomen have the advantage to offer to the patient apart from the reconstruction of a natural breast, the reduction of the excess accumulated abdominal flap typically presented in middle aged patients, with a final result completely similar to an abdominoplasty. Moreover, the location of these flaps allow the performance of the operation without the need of changing the patient's position and as a result, two surgical teams can work contemporaneously, leading to a reduction of the surgical times. More specifically, the DIEP flap permits the complete sparing of the muscular wall in comparison to the free or pedicled TRAM flap that include the whole or a part of the Rectus Abdominis muscle, exposing thus the patient in an increase risk of abdominal hernia, posture problems, increased hospital stay, and a long rehabilitation. Finally, the use of autologous tissues for the reconstruction of the breast, requires more invasive operations that lead to a prolonged hospital stay, a long rehabilitation, and it requires a more organized and qualified hospital (capacity to perform microsurgery), something that is not always available.
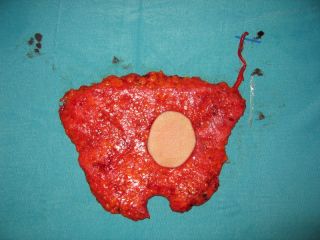
"DIEP" flap (Deep Inferior Epigastric Perforator): consists of the transfer in the thoracic region of a lozenge of cutaneous-adipose or only adipose tissue, taken by the infra-umbilical part of the abdomen through the isolation of the infra-umbilical perforators of the Deep inferior epigastric artery and vein, leaving in place the Rectus abdominis muscle. The epigastric donor vessels are then, anastomosed microsurgically with the prepared recipient vessels that are usually the Thoracodorsal or Internal Mammary artery and vein. At the end, at the donor site, it is left only a scar similar to the one after an abdominoplasty, while in the breast region only a scar that its size and form depends at the dimensions of the skin removed after the mastectomy.
"TRAM" free flap (Transverse Rectus Abdominis Muscolocutaneous): consists of the transfer in the thoracic region of a lozenge of musculocutaneous-adipose or only musculo-adipose tssue, taken by the infra-umbilical part of the abdomen and including the distal part of the Rectus Abdominis muscle that is vascularized by the infra-umbilical perforators of the Deep inferior epigastric artery and vein. Also in this case the epigastric donor vessels are anastomosed microsurgically with the prepared recipient vessels that are usually the Thoracodorsal or Internal Mammary artery and vein. At the abdominal and breast region remain scars similar to the ones described above for the “DIEP” flap.
"TRAM" pedicled flap (Transverse Rectus Abdominis Muscolocutaneous): consists of the transfer in the thoracic region of a lozenge of musculocutaneous-adipose or only musculo-adipose tissue, taken by the infra-umbilical part of the abdomen. The difference between this and the one mentioned above is that this flap includes the proximal part of the Rectus Abdominis muscle through which the flap receives its vascularization from the infra-umbilical perforators of the Inferior Epigastric vessels that anastomose with the Superior Epigastric artery and vein. In this case it is not necessary neither a microsurgical anastomosis of the donor Superior Epigastric vessels, nor the isolation of the recipient vessels. At the abdominal and breast region remain scars similar to the ones described above for the “DIEP” flap.
"Wise pattern": this method consists of the application of the reduction mammaplasty principles for the breast reconstruction. It is possible to use this technique when a quadrantectomy/tumorectomy is indicated, and the part of the breast to be removed corresponds with the one that is usually removed after a reduction mammaplasty, the QIE, QII or the intersection of the QS. After this operation the result will be a periareolar scar, a scar linking the areola and the inframammary fold, a scar along the inframmammary fold and finally a conical breast form completely similar at the one after an esthetic reduction mammaplasty.
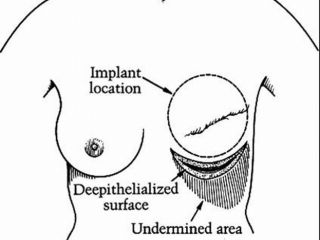
"Modified Wise pattern": this method consists of the modification of the reduction mammaplasty principles in order to adapt it for the breast reconstruction. It is necessary to use this modified technique when there is an indication for a quadrantectomy/tumorectomy, and the part of the breast to be removed does not corresponds to the one removed after a reduction mammaplasty but is the QS. Therefore, it must be preserved a certain quantity of breast tissue and skin of the inferior quadrant ipsilaterally in order to reintegrate it at the removed superior quadrant. After this operation the result will be a periareolar scar, a scar linking the areola and the inframammary fold, and one depending on the case at the SI or SE quadrant. The resulting breast form will be similar to the one after an esthetic reduction mammaplasty.
Implants
The use of implants has the advantage of not making use of autologous tissues, thus reducing the operating times, and the physical stress imposed on the patient but at the same time increasing the need of follow up surgeries in order to achieve a full reconstructive result. In patients with small breasts these methods offer the possibility to perform at the same time an augmentation mammaplasty at the controlateral breast.
The main disadvantage in the use of implants is the incompatibility with radiotherapy, because it leads to necrosis of the skin envelope and the loss of the implant. It is true that with this technique there are no more resulting scars on the breast region, at the same time though it is not possible reconstruct a breast with a certain natural ptosis, therefore in order to achieve a valid symmetry it is needed a reduction mammaplasty or mastopessy on the controlateral breast.
Finally another disadvantage that is usually manifested when a monolateral reconstruction is performed, is the gradual more or less slow loss of symmetry, since the controlateral breast continues ageing thus becoming more ptotic and atrophic while the reconstructed one remains more or less stable in time. The Wise pattern techniques that include the preservation of the cutaneous flaps similar to the ones of reduction mammaplasty, because of the rapport between their thickness and length, present an elevated risk of cutaneous necrosis with loss of the implant and failing of the reconstruction process.
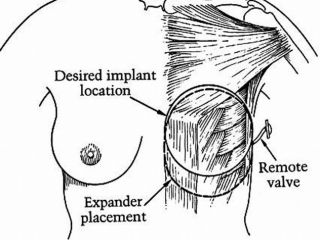
“Tissue Expander and implant”: this reconstructive technique is performed in two operative stages, in the first one together with the mastectomy the tissue expander is positioned and is later filled with 10% of its volume on a weekly basis leading to the needed increase of the skin surface in order to perform the breast reconstruction. After having achieved an appropriate expansion, with an overcorrection of the defect, the second operation is taking place with the substitution of the tissue expander with the implant, that is going to be of a certain volume enough to reconstruct the breast symmetrical to the controlateral one
“Wise pattern + implants”: consists of the application of the reduction mammaplasty principles for the breast reconstruction. It is very similar to the Wise Pattern with autologous tissue with the only difference being the complete removal of the breast gland and the spairing of the skin following the reduction mammaplasty pattern. The breast volume is restored by the use of an implant. The resulting scars will be a periareolar one, a scar linking the areola with the inframammary fold, and a scar along the inframmary fold, similar to the ones after a reduction mammaplasty and thus covered by the bra.
"Modified Wise pattern + implant”:similar to the tecnique described above with the only difference that the skin excised with the tumor is located on the QS and in order to obtain the covering of the implant it is needed to apply a modified reduction pattern.
Autologous tissues and implants
“Lateral Thoracic flap + implant”: consists of the restoration of the cutaneous surface by means of the rotation of a fascio – cutaneous flap originating from the lateral thoracic surface, while for the reconstruction of the breast volume it is used an implant that is positioned under the Pectoralis Major muscle after the dissection of its distal sternal insertion. The resulting scars are one of an upside down V on the breast cone and a horizontal one on the lateral thoracic wall both hidden under the bra.
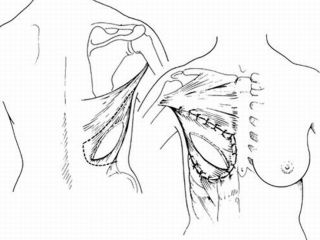
“Latissimus Dorsii with or without implant”: consists of the restoration the cutaneous surface by means of the rotation of a musculocutaneous flap originating from the posterior thoracic surface and, if necessary, the restoration of the breast volume by means of an implant positioned under the Pectoralis Major and Latissimus Dorsi muscle. The resulting scars are an elliptical one on the breast region and one on the posterior thoracic region both hidden under the bra.
Surgical Indications
Autologous tissues
Breast reconstruction with “DIEP” flap is indicated when:
-
A donor area of autologous tissue from the abdomen enough to restore the breast volume is available.
-
Reconstruction of a voluminous breast without the need to do controlateral symmetrization is planned.
-
Pre- or post-operative radiotherapy treatment is planned
-
Reconstruction with implants has previously failed
-
A radical mastectomy with wide excision of soft tissues is planned
The reconstruction with the free or pedicled “TRAM” flap has the same indications as the DIEP flap
Breast reconstruction with “Wise pattern” is indicated when:
-
There is a voluminous breast and at the same time the benefit of a controlateral reduction mammaplasty is considered
-
A quadrantectomy/tumorectomy in the QIE, QII, intersection of the QS quadrants is planned
-
A radiotherapy treatment post-operatively is planned
Breast reconstruction with “Modified Wise pattern” is indicated when:
-
There is a voluminous breast and at the same time the benefit of a controlateral reduction mammaplasty is considered
-
A Quadrantectomy/tumorectomy in the QSE, QSI is planned
-
A radiotherapy treatment post-operatively is planned.
Implants
Breast reconstruction with “expander + implant” is indicated when:
-
A donor site of autologous tissue (p.e abdomen) ideal to tranfer a flap is not available.
-
Radiation therapy is not planned
-
Reconstruction of a small breast is planned and an augmentation mammaplasty of the controlateral breast is desired.
Breast reconstruction with “Wise pattern + implant” “Modified Wise pattern + implant” is indicated when:
-
A skin sparing mastectomy is planned
-
There is a voluminous breast and the benefit of a controlateral reduction mammaplasty is considered.
Autologous flap + implant
Breast reconstruction with “lateral thoracic flap + implant” is indicated when:
-
A donor site of autologous tissue (abdomen) is not availabe
-
A reconstruction of small breast is planned
-
The patient would prefer reconstruction in a single operation
-
The patient accepts a controlateral (reduction mammaplasty) symmetrization
Breast reconstruction with “latissimus dorsi flap + implant” is indicated when:
-
A donor area of autologous tissue (abdomen) that is enough to reconstruct the breast without the use of an implant is not available
-
Reconstruction of a moderate size breast is planned
-
The patient accepts a controlateral (reduction/augmentation mammaplasty) operation
-
Pre- or post- operative radiotherapy treatment is planned
-
Bilateral reconstruction is planned.
Contraindications
Autologous tissues
Breast reconstruction with “DIEP” flap is contraindicated when:
-
The patient has a high ASA index or refuses a long operation (6 hours)
-
The scars of previous operations have interfered with the abdominal vascularization, not permitting the raising of the DIEP flap
-
The patient has a coagulation defect
The reconstruction with the free “TRAM” flap has the same contraindications like the DIEP flap and also the disadvantage to create a muscular defect on the abdominal wall, increasing thus the risk of an abdominal hernia and an increase hospital stay.
The reconstruction with the pedicled “TRAM” flap has the same contraindications like the DIEP flap and the disadvantage to create a muscular defect on the abdominal wall bigger that then free “TRAM” flap, increasing the risk of an abdominal hernia and a long hospital stay.
Breast reconstruction with “Wise pattern” and “Modified Wise pattern” is contraindicated when:
-
Breasts of small sizes are present
-
Patient refuses symmetrization on the contralateral breast
-
An excision wider than a quadrantectomy/tumorectomy is planned.
Implants
Breast reconstruction with “tissue expander + implant” is contraindicated when:
-
Pre- or post- radiotherapy treatment is planned
-
In case of a radical mastectomy (sec. Halsted), including the skin and the pectoral muscles
Breast reconstruction with “Wise pattern + implant” or “Modified wise pattern + implant” is contraindicated when:
-
Pre- or post-radiotherapy treatment is planned
-
Patient refuses symmetrization on the controlateral breast
Autologous flap and implant
Breast reconstruction with “Lateral thoracic flap + implant” is contraindicated when:
-
Pre- or post-radiotherapy treatment is planned
-
Patient refuses symmetrization on the controlateral breast
Breast reconstruction with “Latissimus Dorsi with or without implant” is contraindicated when:
-
There is a vascular or nervous injury of the Latissimus Dorsi flap
-
Patient refuses symmetrization on the controlateral breast.
Preoperative assessment
The week before the operation the patient is advised to avoid any contact with persons that have a cold or any other infectious disease; and to avoid taking any aspirin that will reduce the capacity of blood to coagulate and as a result could provoke excessive bleeding and the formation of hematomas. In addition, the operation should not take place during menstruation. Other than the routine controls for the main disease, a clinical exam, few laboratory exams, an x-ray of the thorax and an ECG are the only exams necessary preoperatively. For patients undergoing reconstruction with the use of microsurgery it is necessary to have them pre-deposit one or two units of their own blood in order to dilute the remaining circulating blood and eventually having it available to transfuse if necessary afterwards. Moreover, it is necessary to perform few months before surgery an ultrasound of the breast or a mammography in order to exclude the presence of any recurring disease of the breast gland that demand a biopsy and histological exam. The patient needs to buy and bring to the hospital in order to use after the operation a soft, elastic sport bra that will be the only bandage used postoperatively. Right before the anesthesia the measurements and designing of the patient are performed, an important part of the preparation of the patient for surgery, that will be used during the operation as a guide for the incisions.
topSurgical techniques
Autologous tissues
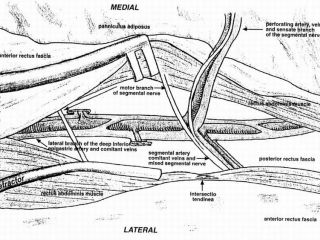
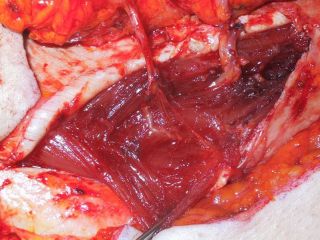
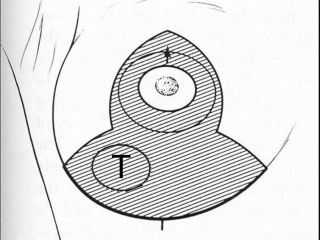
"DIEP" flap (Deep Inferior Epigastric Perforator): the first step is to evaluate the required skin and adipose tissue that is needed to be taken by the abdomen in order to reconstruct the breast with a volume and a ptosis similar to the controlateral one. The quantity of the transferred skin will determine the ptosis and the position symmetry while the quantity of the adipose tissue will determine the volume symmetry. Proceeding, the exact dimensions of the skin that is excised or going to be excised with the breast are projected on the abdominal skin, underneath the umbilicus; and in an empirical way, taking always in consideration that the part removed has a flattened conical form diverse than the abdomen which presents its greatest thickness near the umbilicus, it is evaluated the necessary quantity of adipose tissue that needs to be taken. Their ratio varies, depending on the quantity of skin that is spared with the mastectomy, sometimes having to use a flap made only of adipose tissue like when a subcutaneous mastectomy is performed. The flap is designed in a paramedian position according to the side the vascular pedicle is isolated, and since the flap needs to be rotated 180° it will be ipsilateral to the defect if the Internal Mammary vessels are going to be used for the anastomosis or controlateral if the Thoracodorsal vessels are used. There is a dispute concerning which vessels are better to use for the anastomosis and although a clear answer does not exist to this question, the Thoracodorsal vessels are easier to use in immediate reconstructions since they are exposed during the lymphadenectomy and on the other hand for the delayed reconstructions the Internal Mammary vessels are preferred since the Thoracodorsal ones are near scarring tissue or have suffered damage from radiation. An incision is performed along the design, arriving until the abdominal fascia and in this way along the suprafascial plane the half of the flap far from the pedicle is raised by selecting and ligating the epigastric perforators up to the linea alba. Next, the remaining part of the flap is raised in a latero-medial direction, respecting the paraumbilical perforators that arise by the Deep Inferior Epigastric artery and vein (See Figure) (See Figure).One, two or sometimes three neighbor perforators are selected depending on their volume and the volume of the flap that is going to be transferred, and only the part of the Rectus abdominis muscle that is found among them is sacrificed; the dissection of the perforators is performed following their course intramuscularly until their origin deep inside the pelvis until the iliac vessels (See Video) (See Video) (See Video). The flap is transferred to the breast region and is stabilized by few deep subcutaneous sutures only after the recipient vessels have been prepared, in case of the Internal Mammary vessels the sternocostal cartilage part of the IV rib has to be removed and then their isolation is performed. Only after this step the microsurgical part begins that includes the performance under the microscope of the vascular anastomosis, usually termino-terminal, between the recipient Thoracodorsal or Internal Mammary artery and the Deep Inferior Epigastric Artery and their respecting veins. After having secured the vascular flow, the positioning of the flap is completed. Contemporaneously with the transferring and rivascularization of the flap, the closing of the donor area is performed following the principles of the abdominoplasty, by raising the remaining abdominal superior flap and moving it forward towards the pubis, repositioning the umbilicus through a buttonhole incision. After having placed the suction drains a compressive bandage of only the abdomen, and not of the neo breast, is performed. (see picture) (see picture) (see picture) (see picture) (see picture) (see picture) (see picture) (see picture) (see picture).
"See video on Breast Reconstruction with DIEP Flap"
Free “TRAM” flap (Transverse Rectus Abdominis Muscolocutaneous): The programming of the flap and its transfer to the thoracic region is completely the same with the reconstruction by means of DIEP flap. The only difference concerns the raising of the flap that together with the cutaneous-adipose tissue also the distal part of the Rectus Abdominis muscle is used and as result the intramuscular dissection of the perforators is not needed. The free TRAM flap is also vascularized by the Deep Inferior Epigastric artery and vein. At the same time even the closing of the donor area is the same like the one performed when the DIEP flap is used.
Pedicled “TRAM” flap (Transverse Rectus Abdominis Muscolocutaneous): the programming of the flap and its transfer to the thoracic region is completely the same with the reconstruction by means of DIEP flap. The only difference concerns the raising of the flap that together with the cutaneous-adipose tissue also the proximal supraumbilical part of the Rectus Abdominis muscle. The flap is pedicled proximally and receives its vascularization through the intramuscular anastomosis of the Superior Epigastric Artery and vein and the infraumbilical perforators of the Deep Inferior Epigastric vessels. In this case it is not needed the microsurgical part and the flap is rotated 180° and is transferred to its final location through a subcutaneous tunnel near the inframammary fold. The closing of the donor area is the same like the one performed when the DIEP flap is used.
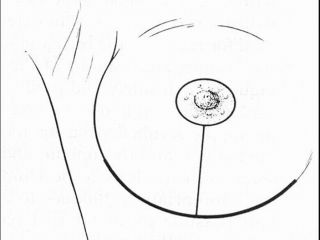
“Wise pattern”: After locating the tumor, and if it is located in the inferior quadrants or cranially at the NAC, it is designed on the breast skin the pattern of the Reduction mammaplasty and the operation proceeds like performing a Reduction mammaplasty. If the tumor is located on the QIE, QII the inferior quadrants are excised, maintaining the vascularization of the NAC through a supero-lateral or supero-medial pedicle (see picture) (see picture). In case of a tumor located cranially, the vascularization of the NAC is preserved through an inferior pedicle and the rest of the gland is removed. At the end the breast is sutured in exactly the same way like after a Reduction mammaplasty (see picture) (see picture).
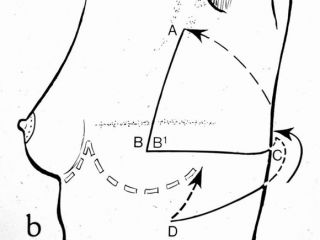
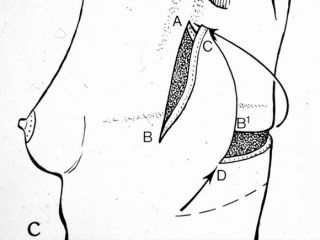
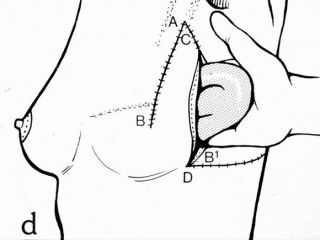
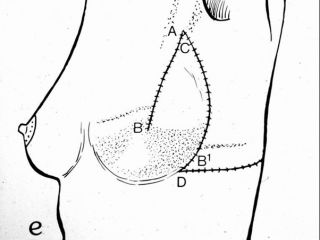
“Modified Wise pattern”: After locating the tumor, and if the sector to be excised with the tumor interests the SI or SE, it is designed on the breast skin the pattern of the modified reduction mammaplasty and the operation proceeds like performing a reduction mammaplasty. The modification concerns the sparing in the corresponding inferior quadrant, of a quantity of skin and breast gland ideal to restore the excised tissue superiorly. The vascularization of the NAC will be preserved through an inferior or superior pedicle opposite to the excised sector. At the end the breast is sutured in exactly the same way like after a Reduction mammaplasty.
Implants
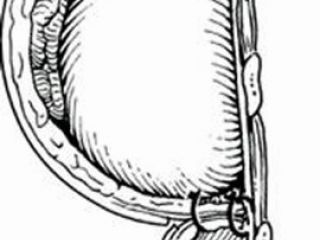
“Expander and implant”: This method includes two surgical steps, during the first one, which is usually performed contemporaneously with the mastectomy, the tissue expander is put in place; its size is chosen by taking into consideration the ones of the controlateral breast (see picture). The tissue expander is placed in a submuscular pocket, created by the Pectoralis major muscle and the Anterio Serratus muscle (see picture). Only after the Pectoralis Major muscle is raised medially, its inferior costosternal insertions are cut and the Anterior Serratus muscle is raised laterally from the costal plane in such a way to create a sufficiently big pocket to place the expander; finally the two muscles are sutured together followed by the skin, leaving in place suction drains. During the operation the tissue expander is filled in order to reduce the dead spaces, while later on it will be filled with a weekly frequency and almost 10% of its volume is added each time until reaching its final volume. By doing this, an increase in the cutaneous thoracic surface necessary to reconstruct in a second surgical time the breast. After the right expansion is reached in order to overcorrect the defect, we proceed in a second surgical time to the removal of the expander by accessing it through the previous scar and its substitution with the definitive implant (see picture), that will be of an ideal volume so as to reconstruct a breast similar to the controlateral one (see picture) (see picture). In order to reach a valid symmetry we often need to perform a reduction mammaplasty or a mastopexy in order to adapt the controlateral breast, sometimes it needs to be repeated in the following years.
“Wise pattern + implant”: the pattern of the reduction mammaplasty is designed on the skin in order to perform a partially subcutaneous mastectomy, that spares the skin included in the pattern of the reduction mammaplasty. Inferiorly, a dermo-adiposous flap is spared that is later sutured superiorly with the Pettoralis major muscle, which has been previously cut medially, in order to create a pocket big enough and define better the inframammary fold. Inside the pocket created the implant is placed. The cutaneous flaps are placed over and they are sutured in the same way like the one of the reduction mammaplasty. The NAC are reconstructed later one. This method is often accompanied by a reduction mammaplasty on the controlateral breast or it can be performed bilaterally, as for example in prophylactic subcutaneous mastectomies (see picture) (see picture).
“Modified wise pattern + implant”: Similar to the technique described above, with the only difference regarding the skin to be excised. The pattern that is applied is a modified one in order to have the excision of the skin in continuity with the tumor and at the same time achieve the covering of the implant.
“Lateral Thorax flap + implant”: First of all the designing of the inframmamary fold is performed by taking in consideration the controlateral one; further on, the incision lines are designed along the lateral margin of the Pectoralis major muscle, at the end of which, on the lateral face of the thorax, a triangular flap is raised whose base will be positioned at the intersection between the lateral margin of the Pectoralis major muscle and the inframammary fold, two thirds over and one third under it, while the longitudinal axis of the flap will be parallel to the ribs (see picture). The flap is raised in a posterior-anterior sense including the muscular fasciae of the Latissimus Dorsi muscle and the Anterior Serratus muscle, guaranting the vascularization through the inferio-medial intercostal perforators. Afterwards, through the incision along the margin of the Pectoralis major muscle, a pocker under the Pectoralis major muscle is created, by sectioning it medially until the inframammary fold, so as the flap will be sutured with the margin of the Pectoralis major muscle after it has been rotated for 70o (see picture); the implant is then placed in order to reconstruct the breast volume and the suturing is completed (see picture). The resulting scars are an inverted V on the breast and a horizontal one on the lateral thoracic wall both hidden by the bra (see picture) (see picture) (see picture).
“Latissimus Dorsii flap + implant”: First of all we need to evaluate, by looking at the controlateral breast, the dimensions of the skin island necessary to transfer on the breast to be reconstructed, which at the end will determine the ptosis and symmetry of the reconstructed breast. Moving on, the design is transported on the back and the exact same dimensions, of the excised skin island, are designed keeping in mind the fact that the flap will have a greater thickness due to the progressive atrophy of the muscle; the volume of the implant needed is evaluated by comparing it to the controlateral breast. The flap is raised by isolating its proximal heard until its origin without dissecting it and by sparing the vascular pedicle; the thoracodorsal nerve is cut. Together with skin island the Latissimus Dorsi muscle, enough to completely cover the implant, is transported ventrally (see picture). After the transfer, the donor area is sutured and closed by first intention, leaving in place a suction drain. The resulting scars will be an elliptical breast scar on the breast and one on the posterior thoracic wall, both hidden under the bra (see picture) (see picture).
"Show video on Breast Reconstruction with Latissimus Dorsi Flap"
topPostoperative treatment
Right after the operation the patient will have to remain for 30 minutes in the observation room, where it will be controlled by the anesthesiologists before she can be permitted to return to her room. General anesthesia could have certain adverse effects such as vomiting, chills, and the patient is allowed to drink small quantities of water only the day after, and therefore the patient will not have dinner but can have breakfast the day after. It is necessary to remain in bed until the morning after. At the patient they will be administered antibiotics in order to prevent any infectious complications and through an infusor they will be administered the analgesics until the end of the first postoperative day, in order to avoid any pain. Like this, the patient should have a calm night under the constant control by the nurses who will be in direct contact with the surgeon. After eight-ten days, at the patient will be given the permission to return at home as soon as the final control is performed by the surgeon who will perform the final bandaging and dressing with the bra, the prescription of the antibiotic and analgesic therapy to continue even while at home. Right after the operation the patient needs to wear an abdominal elastic bandage for 30 days which will then be allowed to remove only during night time and keep for other 30 days when awake. The first medication will be performed after 3-5 days. Only after the removal of the drains the patient will be allowed to have a shower and change immediately the bandage. The sutures will be partially removed after one week and completely after two weeks. Work and social activities should be suspended for at least 30 days after the operation. If the work of the patient is such to demand an increase physical activity (raising weights etc), it will be necessary a longer period of abstinence. The patient can return to its daily physical activities only after the first 15 days postoperatively. Driving and sporting activities can be retaken with caution only two months after the operation. At the beginning a sensation of tension and weight will be felt on the breast region that will appear a bit bigger and located higher than expected, but after 3-6 months it will be at its natural position and size and without this strange sensation. The breasts are never perfectly symmetrical neither during puberty nor afterwards and as result a mild asymmetry, more pronounced initially, after the reconstruction should not be excluded. Such a situation could depend on the unfavorable anatomic/vascular conditions due to previous operations and often could be corrected with small operations performed in local anesthesia. At the donor area (abdomen) the resulting linear scar will be greater than the elliptical cutaneous island that is transferred. Instead, in the breast region despite the efforts to hide the resulting scars, some of them will be more visible according to the type of the mastectomy chosen. Finally, the quality of the scars cannot be predicted and will depend on the personal healing characteristics of the patient.
topComplications
Bleeding is very rare (0.5%), but can present only during the first 12 hours after the operation and does not depend on the ability of the surgeon; in such a case it will be necessary to return to the operating room for a 30-60 minutes operation in order to control it. This complication, if it is managed well, will not provoke other inconveniences and it will not prolong the hospital stay.
Infection, thanks to antibiotics, is very rare, but if present, can lead to the loss of the implant and a waiting time of few weeks or months in order to repeat the operation.
Total necrosis of the flap, even if it is very rare (1-2%), it can more frequently be presented in smokers, patients that have undergone radiation therapy, the elderly and those that have an history of numerous operations. This can depend on the obstruction of the executed vascular anastomosis in order to revascularize the flap. The reasons why it happens are various, like the quality of the vascular wall, the blood coagulation, unfavorable anatomic conditions of the vascular pedicle. Thanks to the continuous control after the operation, the obstruction is noticed immediately and the surgeon can intervene and resolve the situation immediately. Moreover, it can happen that the perfusion of the flap is not clear, or it is impossible to restore the flow and therefore it will be necessary the removal of the flap by the breast. This event, that will indicate the failure of the reconstruction, does not put the patient’s life into risk and the patient can still conserve the aesthetic result of the abdomen and after 6 months a new plan should be made in order to find an alternative method that will offer satisfying results.
Partial necrosis of the flap is rare (5-7%), and it is only a represented by a peripheral hardening of the adipose tissue transferred from the abdomen and/or by a loss of part of the skin. Its frequency increases (15%) if part of the flap is the 4th zone, of high perfusion risk, and by means of a clinical exam or an ultrasound it can be diagnosed and which nevertheless does not present a clinical problem. Rarely, it is necessary to perform a revision, in local or general anesthesia depending on the problem but in most cases it is not necessary to do anything. In most cases the esthetic result is satisfying.
topBibliography (Search on pubmed)
-
Allen RJ, Treece P. Deep inferior epigastric perforator flap for breast recostruction. Ann Plast Surg 32(1): 32-8, 1994.
-
Arnez ZM, Khan U, Pogorelec D, Plannisek F. Breast reconstruction using the free superficial inferior epigastric artery (SIEA) flap. Br J Plast Surg 52: 276-279, 1999.
-
Berrino P, Santi P. Preoperative TRAM flap planning for postmastectomy breast reconstruction. Ann Plast Surg, 21(3): 264-72, 1988.
-
Blondeel Pn, Boeckx WD. Refinements in free flap breast reconstruction: the free bilateral deep inferior epigastric perforator flap anastomosed to the internal mammary artery. Br J Plast Surg 47(7): 495-501, 1994.
-
Blondeel N, Wanderstraeten GG, Monstrey SJ, Van Landuyt K, Tonnard P, Lysens R, Boeckx WD, Matton G. The donor site morbidity of free DIEP flaps and free TRAM flaps for breast reconstruction. Br J Plast Surg 50(5): 322-30, 1997.
-
Boyd JB, Taylor GJ and Corlett R. The vascular territories of the superior epigastric and the deep inferior epigastric systems. Plast. Reconstr. Surg. 73:1, 1-14, 1984.
-
Gill PS, Hunt JP, Guerra AB, Dellacroce FJ, Sullivan SK, Boraski J, Metzinger SE, Dupin CL, Allen RJ. A10-Year Retrospective Review of 758 DIEP Flaps for Breast Reconstruction. Plast. Reconstr. Surg. 113:4, 1153-1160, 2004.
-
Hartrampf CR, Scheflan M, and Black PW. Breast reconstruction with a transverse abdominal island flap. Plast. Reconstr. Surg. 69:216, 1982.
-
Holmstrom H. Lossing C. The lateral thoracodorsal flap in breast reconstruction. Plast Reconstr Surg. Jun;77(6):933-43,1986.
-
Holmstrom H. The free abdominoplasty flap and its use in breast reconstruction. An experimental study and clinical case report. Scand J Plast Reconstr Surg 13(3); 423-27, 1979.
-
Koshima I, Soeda S. Inferior epigastric artery skin flaps without rectus abdominis muscle. Br J Plast Surg 42(6): 645-8, 1989.
-
Koshima I, Moriguchi T, Soeda S, Tanaka H, Umeda N. Free thin paraumbilical perforator based flap. Ann Plast Surg 29(1): 12-7, 1992.
-
Kroll SS, Reece GP, Miller MJ, Robb GL, Langstein HN, Butler CE, and Chang DW. Comparison of cost for DIEP and free TRAM flap breast reconstructions. Plast. Reconstr. Surg. 107:6, 1413-1416, 2001.
-
Moon HK, Taylor GJ. The vascular anatomy of Rectus Abdominis Muscolocutaneous flaps based on the Deep Superior Epigastric System. Plast. Reconstr. Surg. 82:5, 815-829, 1988.
-
F. Santanelli, G. Paolini, L. Renzi.Preliminary experience in breast reconstruction with the free Vertical Deep Inferior Epigastric Perforator flap. Scand J Plast Reconstr Hand Surg. 2008;42(1):23-27.
-
Santanelli F., Paolini G., Campanale A., Longo B., Amanti C. Modified Wise Pattern Reduction Mammaplasty, A New Tool For Upper Quadrantectomies: A Preliminary Report. Ann Surg Oncol. 2009 May;16(5):1122-7.
-
Santanelli F., Paolini G., Campanale A., Longo B., Amanti C.The “Type V” skin sparing mastectomy for upper quadrants skin resections”. Annals of Plastic Surgery. 2010;65(2):135-139.
-
Santanelli F., Paolini G., Amanti C., Longo B., Campanale A. Retrospective analyses of 79 consecutive skin sparing mastectomies type IV: risk factors and complications. Plast Reconstr Surg. 2010;xx(x):xx-xx. In press
-
Santanelli F., Paolini G., Longo B., Angelini M., Laporta R. Prospective computerized analyses of sensibility in breast reconstruction with non-reinnervated DIEP flap. Plast Reconstr Surg. 2010;xx(x):xx-xx. In press